Anti-Muscle-Specific Kinase (MuSK) Antibodies
Test details
Autoantibodies against the acetylcholine receptor (AChR) and muscle-specific tyrosine kinase (MuSK) support the diagnosis of myasthenia gravis and have a pathogenic role in the disease. The autoimmune reaction occurs at the neuromuscular junction, impairing nerve impulse transmission. The hallmark symptom is exertional muscle weakness, asymmetrically affecting specific muscle groups.
Anti-AChR antibodies are highly specific for myasthenia gravis and are found in approximately 85% of patients. Early-onset cases mainly affect women under the age of 40, while late-onset cases (after 50) are more common in men. In approximately 20% of cases, this disorder is limited to the ocular muscles; however, in most patients, it evolves into a generalised form within a few years. Myasthenic crises can be life-threatening due to respiratory muscle weakness and dysphagia.
Approximately 6% of patients with myasthenia gravis are negative for anti- AChR antibodies: about one-third of the latter test positive for anti-MuSK antibodies, which are usually associated with a more severe disease course, predominantly affecting younger women.
Some patients affected by generalised myasthenia gravis test negative for both anti-AChR and anti-MuSK antibodies (double seronegative patients). In these cases, the disease may be caused by other rare autoantibodies.
In patients presenting typical symptoms, the diagnosis of myasthenia gravis is often based on autoantibody testing. Antibody levels against AChR and MuSK correlate well with the clinical picture, although they can vary significantly between individuals. In late-onset forms, the detection of anti-AChR antibodies helps in the differential diagnosis from other diseases with similar symptoms (such as amyotrophic lateral sclerosis (ALS), stroke, Lambert-Eaton syndrome and congenital myasthenic syndrome).
Myasthenia gravis is often associated with other autoimmune diseases. Additionally, approximately 20% of anti- AChR positive adult patients develop a thymoma.
Sample type
Serum, EDTA plasma, heparin plasma, citrate plasma
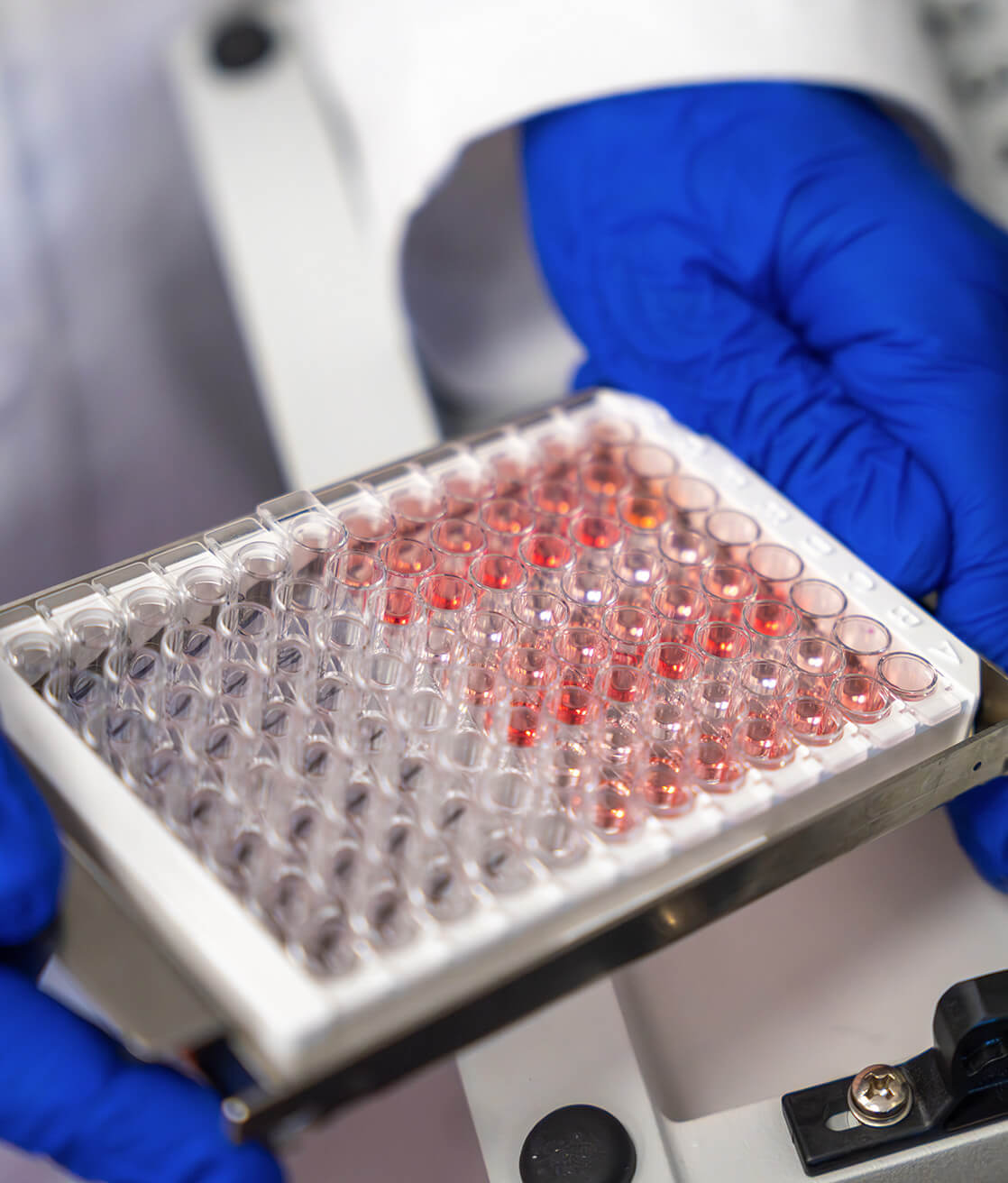
Method
IFA cells
Preparation
Fasting for at least 8-12 hours before sampling
Storage conditions
Refer to the Health Service Charter to check storage conditions
Shipping
+2/+8°C
References
Mirian A, Nicolle MW, Edmond P, Budhram A. Comparison of fixed cell-based assay to radioimmunoprecipitation assay for acetylcholine receptor antibody detection in myasthenia gravis. J Neurol Sci. 2022 Jan 15;432:120084. doi: 10.1016/j.jns.2021.120084. Epub 2021 Dec 8. PMID: 34906880.
Li Y, Arora Y, Levin K. Myasthenia gravis: newer therapies offer sustained improvement. Cleve Clin J Med. 2013 Nov;80(11):711-21. doi: 10.3949/ccjm.80a.13044. PMID: 24186889.
Lazaridis K, Tzartos SJ. Autoantibody Specificities in Myasthenia Gravis; Implications for Improved Diagnostics and Therapeutics. Front Immunol. 2020 Feb 14;11:212. doi: 10.3389/fimmu.2020.00212. PMID: 32117321; PMCID: PMC7033452.
Chan KH, Lachance DH, Harper CM, Lennon VA. Frequency of seronegativity in adult-acquired generalized myasthenia gravis. Muscle Nerve. 2007 Nov;36(5):651-8. doi: 10.1002/mus.20854. PMID: 17654558.

laboratory analysis
Find other tests
Total tau
This test provides the quantitative determination of total tau protein to support the diagnosis of Alzheimer’s disease.
Phosphorylated Tau (pTau181)
This test provides the quantitative determination of tau protein phosphorylated at threonine 181 (pTau181), to support the diagnosis of Alzheimer’s disease.
Anti–NMDAR Antibodies
Test for the determination of human autoantibodies against NMDAR to support the diagnosis of paraneoplastic neurological syndromes with an intermediate-risk phenotype.
Discover what’s new
Subscribe to the newsletter
Subscribe to our newsletter to be always updated.