Anti–Thrombospondin Type-1 Domain-Containing 7A (THSD7A) Antibodies
Test details
Membranous nephropathy (MN) is the most common cause of adult nephrotic syndrome worldwide. Although it occurs predominantly in Caucasian men over 40 years of age, it can affect both sexes and all ethnic groups. The clinical course is variable: while in most cases it regresses spontaneously or remains stable, in about one third of cases it progresses to chronic kidney failure and the risk of end-stage renal disease. In approximately 20% of patients, MN is secondary. For therapeutic purposes, secondary MN must be distinguished from primary (idiopathic) MN (pMN).
The autoimmune mechanisms underlying pMN involve the formation of autoantibodies against the antigens PLA2R and THSD7A. These podocyte surface transmembrane proteins are expressed in human glomeruli. The binding of autoantibodies damages podocytes, allowing proteins to pass into the primary urine. As proteinuria rises, the long-term risk of kidney failure increases, with high morbidity and mortality rates, especially due to thromboembolic and cardiovascular complications.
The diagnosis of pMN is traditionally based on a kidney biopsy with histology and/or electron microscopy. The serological detection of pMN-specific antibodies is faster and less burdensome for the patient.
PLA2R is the main target antigen in pMN. Anti-PLA2R antibodies are highly specific and are detected in up to ~75% of affected patients.
Autoantibodies against THSD7A are detected mainly in pMN patients who are seronegative for anti-PLA2R, representing a second key diagnostic marker in more complex cases, with a prevalence ranging between ~2.5% and 14% in pMN patients. Only rarely do anti-PLA2R and anti-THSD7A occur simultaneously.
Sample type
Serum, EDTA plasma, heparin plasma, citrate plasma
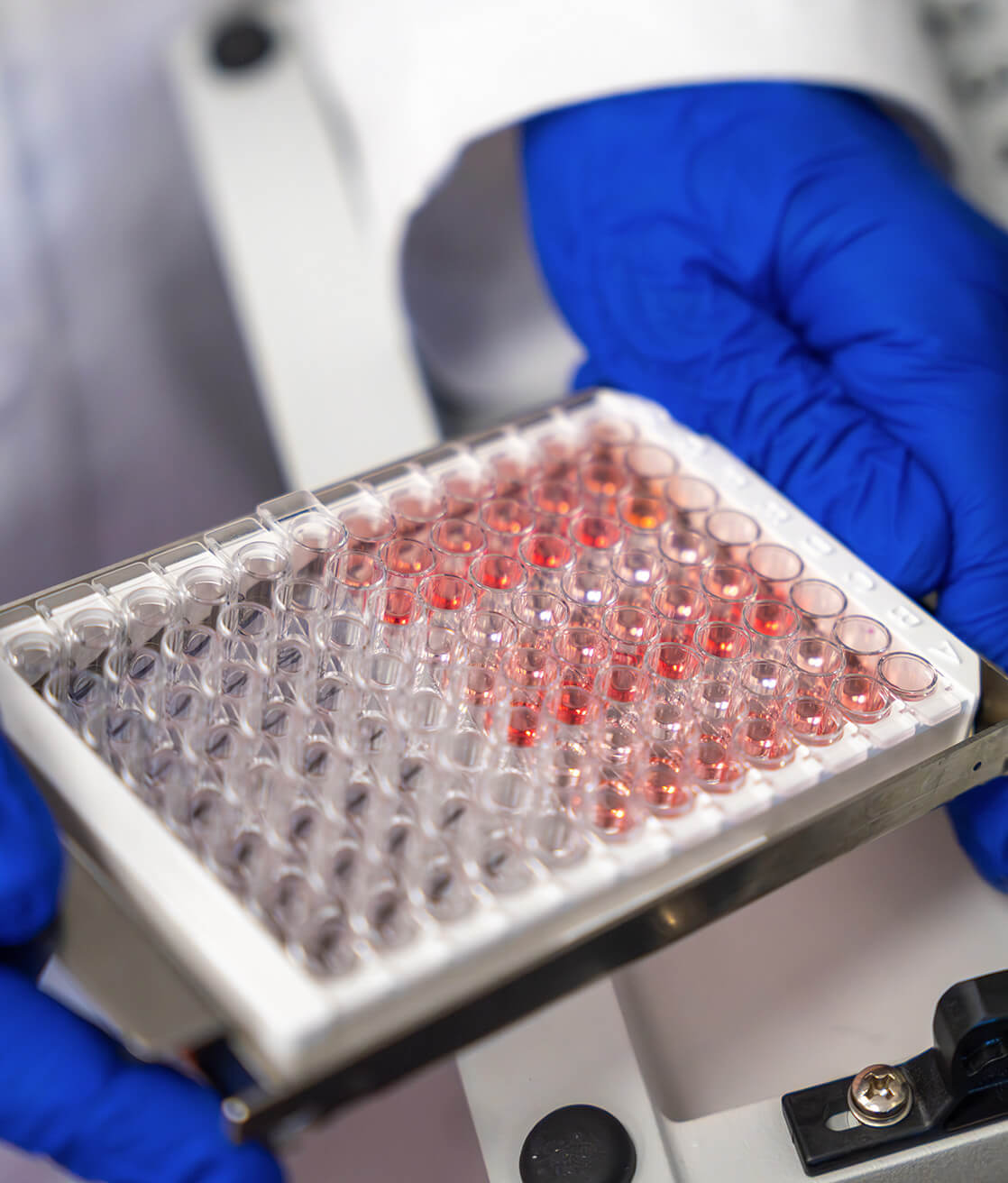
Method
IFA cells
Preparation
Fasting for at least 8-12 hours before sampling
Storage conditions
Refer to the Health Service Charter to check storage conditions
Shipping
+2/+8°C
References
Chen A, Frank R, Vento S, Crosby V, Chandra M, Gauthier B, Valderrama E, Trachtman H. Idiopathic membranous nephropathy in pediatric patients: presentation, response to therapy, and long-term outcome. BMC Nephrol. 2007 Aug 6;8:11. doi: 10.1186/1471-2369-8-11. PMID: 17683621; PMCID: PMC1959515.
Debiec H, Martin L, Jouanneau C, Dautin G, Mesnard L, Rondeau E, Mousson C, Ronco P. Autoantibodies specific for the phospholipase A2 receptor in recurrent and De Novo membranous nephropathy. Am J Transplant. 2011 Oct;11(10):2144-52. doi: 10.1111/j.1600-6143.2011.03643.x. Epub 2011 Aug 9. PMID: 21827616.
Gunnarsson I, Schlumberger W, Rönnelid J. Antibodies to M-type phospholipase A2 receptor (PLA2R) and membranous lupus nephritis. Am J Kidney Dis. 2012 Apr;59(4):585-6. doi: 10.1053/j.ajkd.2011.10.044. Epub 2011 Dec 16. PMID: 22177657.
Hofstra JM, Beck LH Jr, Beck DM, Wetzels JF, Salant DJ. Anti-phospholipase A₂ receptor antibodies correlate with clinical status in idiopathic membranous nephropathy. Clin J Am Soc Nephrol. 2011 Jun;6(6):1286-91. doi: 10.2215/CJN.07210810. Epub 2011 Apr 7. PMID: 21474589; PMCID: PMC3109923.
Hoxha E, Harendza S, Zahner G, Panzer U, Steinmetz O, Fechner K, Helmchen U, Stahl RA. An immunofluorescence test for phospholipase-A₂-receptor antibodies and its clinical usefulness in patients with membranous glomerulonephritis. Nephrol Dial Transplant. 2011 Aug;26(8):2526-32. doi: 10.1093/ndt/gfr247. Epub 2011 Jun 1. PMID: 21633097.

laboratory analysis
Find other tests
Total tau
This test provides the quantitative determination of total tau protein to support the diagnosis of Alzheimer’s disease.
Phosphorylated Tau (pTau181)
This test provides the quantitative determination of tau protein phosphorylated at threonine 181 (pTau181), to support the diagnosis of Alzheimer’s disease.
Anti–NMDAR Antibodies
Test for the determination of human autoantibodies against NMDAR to support the diagnosis of paraneoplastic neurological syndromes with an intermediate-risk phenotype.
Discover what’s new
Subscribe to the newsletter
Subscribe to our newsletter to be always updated.